NOTE: This article originally appeared in Journal of Stem Cell Research & Therapeutics
Coronavirus disease 2019 (COVID-19), a highly contagious disease, is propelled by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). First identified in December 2019 in Wuhan, COVID-19 quickly forced the World Health Organization (WHO) to declare the 2019–20 coronavirus outbreak a Public Health Emergency of International Concern (PHEIC)on 29 January 2020 and a pandemic on 11 March 2020.1-3
Following the emergence, global powers are scrambling in search of reliable treatments urgently, and vaccines for future use. The deathly pathogenic virus has caused more than 3 million cases and two thousand deaths worldwide by April 29th, inciting the fear that the numbers may continue to increase. Common symptoms of COVID-19 include, but are not limited to, fever, cough, fatigue, shortness of breath, and loss of smell sense. Severe additional symptoms included in the list but not limited to are difficulty in breathing, persistent chest pain, confusion, and difficulty in waking up.
While many cases only display mild symptoms, others may manifest a form of viral pneumonia leading to multi-organ failure and could be fatal.4-6
The viral infection causes a vicious release of different proinflammatory cytokines or a cytokine storm thought to be the root cause of organ failures.5 The virus has been recorded to spread between humans following a close contact with someone who has been infected, via small droplets that come from coughing or sneezing. Many humans can also get infected by being even in the vicinity of an infected person or after coming in contact of a contaminated surface and then touching their face.
The standard method of diagnosis and testing used by many countries is the method of real-time reverse transcription polymerase chain reaction (rRT-PCR) from a nasopharyngeal swab. Chest CT imaging is also helpful during the diagnosis stage; however, CDC guidelines do not recommend chest scans for routine screening.
COVID-19 affects the lungs the most, because the virus attacks host cells via the angiotensin-converting enzyme 2 receptor (ACE2). ACE2 is found on the surface of different cell types but type II alveolar cells present in the lungs are very rich in its content. The virus has a surface glycoprotein called a “spike” (peplomer) which helps in accessing the ACE2 and invade the host cell.
Therefore, density of ACE2 in the cells of a tissue is related to the severity of the effect of the infection. Considering its role in infection, many scientists have hypothesized that decreasing ACE2 activity might have positive effects in inhibiting infection. Though an opposing view also exists according to which increasing ACE2 activity by using angiotensin II receptor blocker may be protective. Both of these ideas need to be rigorously tested before either of these could be a guiding force for developing a therapeutic intervention. When the alveolar disease begins to progress, respiratory failure may begin and death may result. The virus also attacks gastrointestinal organs as ACE2 is present.
Currently, there is no available vaccine or specific antiviral treatment for COVID-19. Management involves the treatment of symptoms, supportive care, isolation, and experimental measures. Because of the emergent need, medical professionals have rushed to help the suffering individuals with many already established treatments for pneumonia only to record partial success of recovery. In desperate efforts to find comparatively more efficient treatments, clinicians have tried innovative therapies including stem cell-based one.
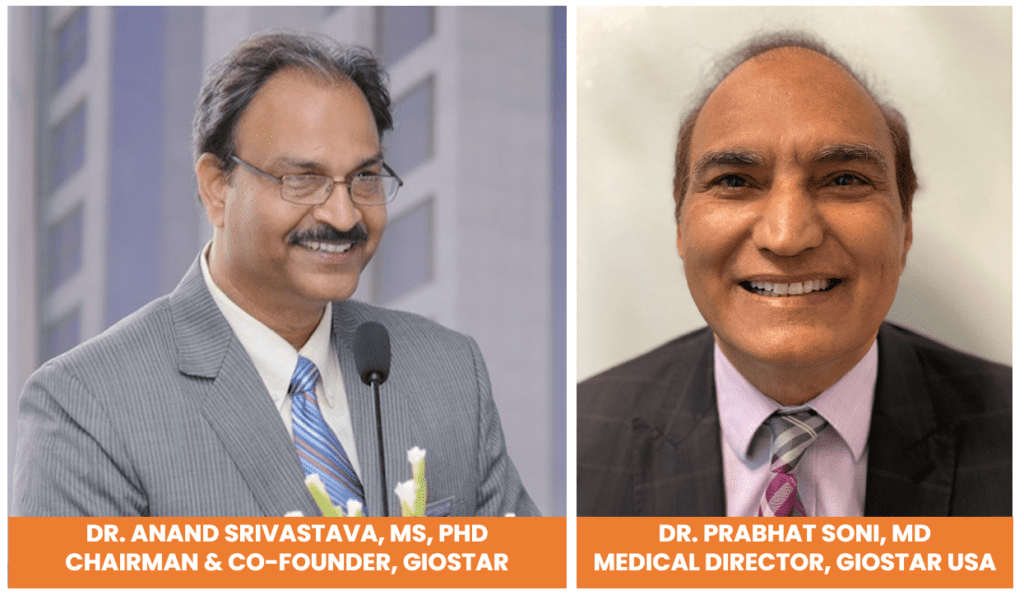
Encouraging findings based on clinical trials in China on COVID-19 patients demonstrate that intravenous infusions of donor mesenchymal stem cells (MSCs) helped recover them. In the light of such few reports the US Food and Drug Administration (FDA) also approved MSC-treatments to be used in the very sickest COVID-19 patients under the clause for expanded access compassionate use and San Diego based GIOSTAR is one of the leading companies to receive the permission.
We assert that “The rationale for approving the stem cells for treating COVID-19 patients is rooted in two facts. The first one is that SARS Cov2 infections provoked uncontrolled immune-response characterized by cytokine release syndrome or cytokine storm. In COVID-19 patients release of very high levels of these pro- inflammatory proteins like IL-6, IL-7 and TNF-alpha push the immune system into overdrive mode and the patient’s own tissues and organs can be damaged sometimes fatally. The second fact is based on the immune-modulatory capacity of MSCs including anti-inflammatory. Therefore, MSCs may help fend off the COVID-19-induced cytokine storm.
Stem cells are found in various organs in the body but the number of resident stem cells can vary significantly among them. These cells are easily prepared from organs having comparatively higher number of these cells like bone marrow or visceral fat from normal individuals and also from tissues like placenta and umbilical cord retrieved after normal births.
On the basis of immuno-modulatory ability, MSCs isolated from donors, called allogeneic cells, and expanded in culture are infused into patients as experimental treatments for a number of different diseases including lung disease like acute respiratory distress syndrome (ARDS) where a build-up of fluids in the lungs results in severe oxygen deprivation. ARDS is a common manifestation of the cytokine storms, and the cause of death in many COVID-19 patients.
Many scientists, on the basis of the immune- modulatory ability of MSCs and other circumstantial evidence, think that MSCs should alleviate the symptoms in COVID-19 patients. It was evident by the Chinese study, which was reported in “Aging and Disease” last month also. The findings based on seven COVID-19 patients who received intravenous infusions of MSCs recovered successfully and were discharged from the hospital by the end of the 14-day observation period. In contrast, of the three patients of the control group receiving regular treatment, all of whom had severe disease, one died, one developed ARDS, and one achieved a stable condition.7,8
Many scientists see that MSCs could be a very promising approach for treatment of COVID-19 patients though the findings are based on a small number of subjects. Other scientists also think that the report demonstrates that the MSCs are not only well received by the patients but also impart a great therapeutic relief. Following the recent approval by FDA of the treatment for extreme cases and trials together with the recruitment of COVID-19 patients to existing MSC trials for ARDS around the world a significant amount of data will demonstrate the therapeutic value of allogenic stem cell-based treatments in COVID-19 patients.
Reviewing all the developing data, we suggest that clinicians may safely use MSCs to manage those patients who are in severe condition. MSCs may also be used as a credible preventive therapy to make the immune system ready to fight the virus in case of any possible COVID-19 infection.
References
- Symptoms of Coronavirus. U.S. Centers for Disease Control and Prevention (CDC).
- Q&A on coronaviruses (COVID-19). World Health Organization (WHO).
- Hopkins, Loss of sense of smell as marker of COVID-19 infection. Ear, Nose and Throat surgery body of United Kingdom.
- Hui DS, I Azhar E, Madani TA, et The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266.
- Puja Mehta, Daniel F McAuley, Michael Brown, et al. COVID-19: consider cytokine storm syndromes and The Lancet. 2020;395(10229):1033–1034.
- “Q&A on coronaviruses”. World Health Organization (WHO).
- Gu Jinyang, Han Bing, Wang COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission”. Gastroenterology.
- Leng Zikuan, Zhu Rongjia, Hou Wei, et al. Transplantation of ACE2-Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia[J]. Aging and disease. 2020;11(2):216–228.
Citation: Soni P, Srivastava A. Mesenchymal stem cells may be a credible alternative therapy to fight with COVID-19 pandemic. J Stem Cell Res Ther. 2020;6(2):79‒80. DOI: 10.15406/jsrt.2020.06.00145

